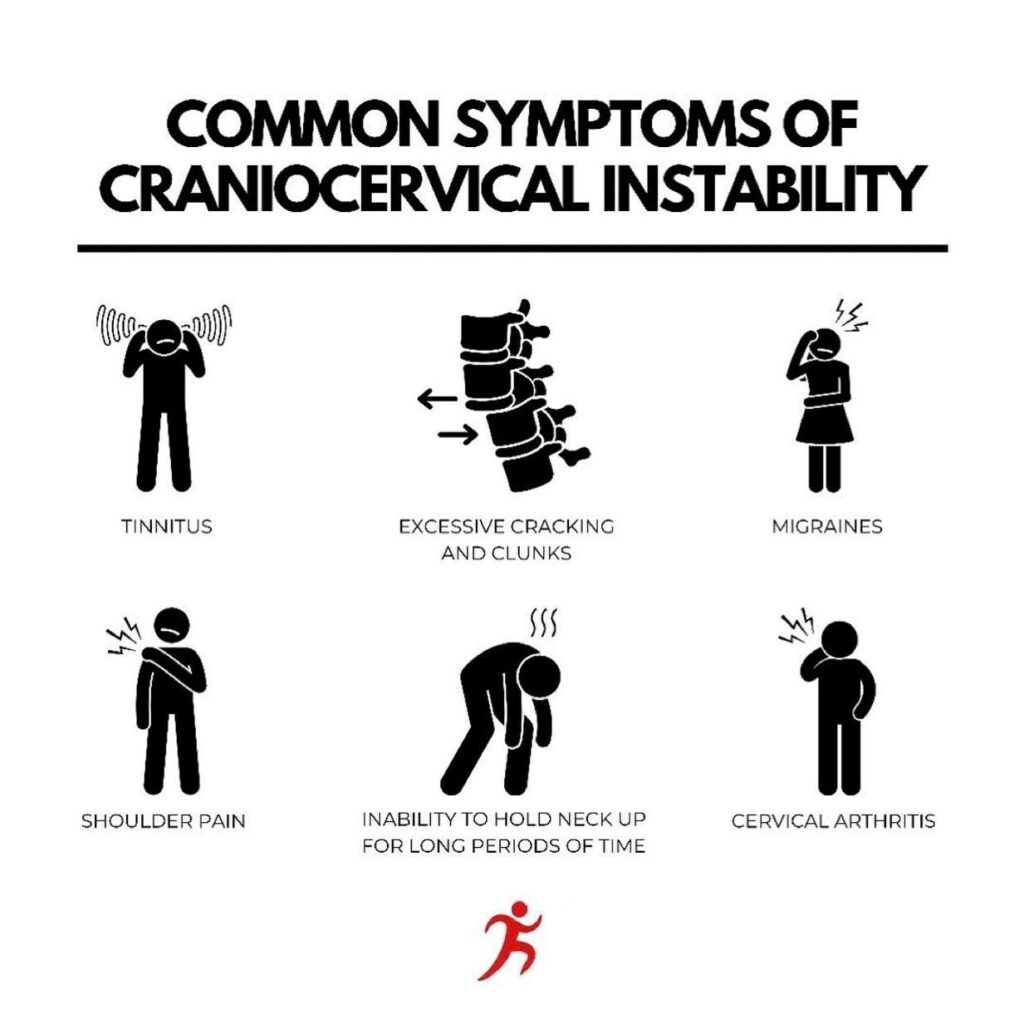
Cervical instability is a complex condition characterized by excessive motion or laxity within the cervical spine. While neck pain and reduced range of motion are commonly associated with cervical instability, this condition can manifest a wide range of symptoms that extend beyond the musculoskeletal system. This article explores the pathogenesis of cervical instability with a focus on the mechanisms underlying various associated symptoms, including anxiety, balance difficulties, cognitive impairment, crepitation, difficulty sleeping, dizziness, drop attacks, dysphagia, ear pain, fatigue, the need to crack the neck, headaches, inability to hold an adjustment, irritability, lightheadedness, memory problems, migraines, muscle tightness/spasms, nausea/vomiting, neck pain/stiffness/soreness, paresthesias, radiating pain into arms and/or shoulders, speech disturbances, temporary relief with a neck brace, tinnitus, vertigo, and visual disturbances.

What is Cervical Instability?
Cervical instability refers to abnormal movement between vertebrae in the neck. This may result from ligament damage, trauma, or degeneration. Patients often ask what cervical spine instability is because it affects posture and movement and causes persistent discomfort.
What Causes Cervical Instability?
Cervical instability causes include trauma, ligament injuries, connective tissue disorders, or degenerative changes. These weaken spinal structures, reducing stability and leading to abnormal vertebral movement, nerve compression, and persistent neck pain over time.
Common Symptoms of Cervical Instability
The signs of cervical instability may include neck pain, stiffness, headaches, dizziness, and difficulty maintaining posture. In severe cases, patients report numbness, tingling, or weakness in the arms, reflecting nerve irritation linked to cervical spine instability.
Anxiety
Anxiety in cervical instability may stem from chronic pain and the uncertainty surrounding symptom exacerbations. Pain-related anxiety can trigger the release of stress hormones, contributing to increased muscle tension and discomfort.
Balance Difficulty, Dizziness, and Vertigo
Balance difficulties, dizziness, and vertigo often result from cervical instability’s impact on the proprioceptive input from cervical structures to the brainstem and vestibular system. Abnormal cervical motion can disrupt sensory input, leading to equilibrium disturbances.
Cognitive Impairment and Memory Problems
Cervical instability can affect cognitive function due to reduced blood flow to the brain or altered cerebrovascular dynamics. Inadequate cerebral perfusion may result from vertebral artery compression or vascular compromise, leading to cognitive impairment and memory problems.
Crepitation
Crepitation, the sensation of grinding or popping in the neck, arises from friction between unstable cervical structures. Ligamentous laxity or facet joint instability can cause abnormal movement and noise generation within the cervical spine.
Difficulty Sleeping and Fatigue
Cervical instability-related pain and discomfort often disrupt sleep patterns, leading to difficulty sleeping and fatigue. Chronic sleep disturbances can exacerbate cognitive impairment, irritability, and overall well-being.
Drop Attacks
Drop attacks, sudden episodes of falling without warning, may result from cervical instability-induced compression or irritation of the spinal cord. Such events can be frightening and pose a risk to patient safety.
Dysphagia
Dysphagia, difficulty swallowing, can occur when cervical instability impairs the coordination of throat muscles. In severe cases, it may result from cervical spine compression affecting the neural control of swallowing.
Ear Pain, Speech Disturbances, and Tinnitus
Cervical instability can lead to referred pain patterns, causing symptoms such as ear pain and speech disturbances. Additionally, nerve compression or irritation in the cervical region may lead to tinnitus, the perception of ringing or noise in the ears.
Headaches and Migraines
Cervical instability can contribute to cervicogenic headaches and migraines through altered cervical biomechanics, nerve irritation, or muscle tension. These headaches often radiate from the neck to the head.
Muscle Tightness/Spasms and Neck Pain/Stiffness/Soreness
Muscle tightness, spasms, and neck pain/stiffness/soreness are direct consequences of cervical instability. Abnormal motion can lead to muscle overuse and irritation, resulting in discomfort.
Nausea/Vomiting
Nausea and vomiting may occur due to the body’s response to pain, anxiety, or cervical instability-induced disturbances in blood flow, especially if vertebral artery compression is involved.
Paresthesias and Radiating Pain
Paresthesias (abnormal sensations) and radiating pain into the arms and/or shoulders often result from nerve compression or irritation in the cervical region. These symptoms can manifest as tingling, numbness, or shooting pain.
Irritability and Lightheadedness
Chronic pain, sleep disruption, and cognitive impairment can contribute to irritability, while lightheadedness may be related to cervical instability-induced alterations in blood flow or autonomic nervous system dysfunction.
Temporary Relief with a Neck Brace
Temporary relief with a neck brace suggests that cervical instability may involve mechanical factors such as excessive motion. Immobilization can alleviate symptoms by restricting motion and reducing irritation.
Visual Disturbances
Visual disturbances may result from alterations in blood flow to the brain, affecting visual processing centers. This can manifest as blurred vision, light sensitivity, or visual disturbances.
How is Cervical Instability Diagnosed?
Diagnosis involves clinical evaluation and imaging tests to confirm abnormal movement. Physicians assess patient history, symptoms, and functional limitations. Advanced imaging is crucial to differentiate instability from other spinal disorders and understand what causes cervical instability effectively.
Imaging: MRI, CT, DMX
MRI evaluates soft tissue, CT provides bone detail, and DMX captures real-time spinal motion. Together, they identify abnormalities associated with craniocervical instability and help clinicians determine the most suitable treatment approach for long-term management of cervical instability causes.
Physical Examination & History
Doctors perform neurological tests, range-of-motion checks, and posture assessments. Patient history is critical in identifying triggers, such as injuries or degenerative disease. Clinical exams complement imaging and reveal early symptoms of craniocervical instability often missed by scans alone.
Cervical Instability Treatment Options
Treatment includes rest, physiotherapy, medications, and sometimes bracing. Physical therapy strengthens supporting muscles, while medications reduce inflammation. In advanced cervical spine instability, regenerative injections or surgical intervention may be considered to restore spinal stability and improve the patient’s quality of life.
When is Surgery Recommended?
Surgery is recommended when conservative care fails or neurological symptoms worsen. Procedures may involve spinal fusion or stabilization techniques, aimed at correcting structural deformities. These approaches address persistent signs of cervical instability and prevent further spinal or nerve damage.
Conclusion
Cervical instability is a complex condition with a diverse array of associated symptoms, extending beyond neck pain and stiffness. The pathogenesis of these symptoms often involves disruption of normal cervical biomechanics, nerve compression, altered blood flow, and neurological dysfunction. Understanding the mechanisms underlying these symptoms is essential for comprehensive evaluation and management of cervical instability. Effective treatment strategies should address the underlying causes of instability and target symptom-specific interventions to improve the patient’s overall quality of life.
References
Image taken from https://www.facebook.com/ActifyPT/photos/ a.1908082926002201/ 2678982515578901/ ?type=3
FAQs About Cervical Instability
Early signs include neck pain, stiffness, difficulty holding posture, muscle spasms, and mild headaches. Some patients also experience dizziness or tingling in the arms, reflecting early neurological involvement.
Yes, cervical instability may cause headaches and dizziness. Abnormal spinal movement can compress nerves or blood vessels, leading to impaired circulation, balance issues, and pain radiating into the head and shoulders.
Craniocervical instability diagnosis involves patient history, physical examination, and imaging tests such as MRI, CT, or DMX. These confirm abnormal movement, detect soft tissue damage, and assess structural alignment in the neck.
The best treatment depends on severity. Conservative options include rest, physiotherapy, medications, and bracing. Advanced cases may require regenerative therapies or surgery to stabilize the spine and prevent neurological complications.
Yes, many cases improve without surgery through physical therapy, strengthening exercises, posture correction, and anti-inflammatory medications. Non-surgical treatments can restore function, reduce pain, and prevent worsening of cervical spine instability.