Detailed Mechanisms, Indications & Contraindications of Medicines, Interventional Pain Management & Regenerative Therapies
Neck pain is not a single disease—it is a symptom arising from different pain generators such as muscles, ligaments, facet joints, intervertebral discs, nerve roots, or cervical instability.
At Alleviate Pain Clinic, treatment selection is mechanism-based, ensuring each therapy addresses the actual source of pain rather than offering temporary suppression.
Below is a detailed, clinician-level explanation of every modality used.
I. Medicines for Neck Pain – Detailed Mechanism, Indications & Contraindications

1. Paracetamol (Acetaminophen)
Mechanism of Action
- Acts centrally by inhibiting prostaglandin synthesis in the brain
- Alters pain perception without significant anti-inflammatory action
Indications
- Mild to moderate neck pain
- Early-stage muscular strain
- Patients who cannot tolerate NSAIDs
Contraindications
- Chronic liver disease
- Alcohol dependence
- Overdose risk with prolonged high doses
2. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Mechanism of Action
- Acts centrally by inhibiting prostaglandin synthesis in the brain
- Alters pain perception without significant anti-inflammatory action
Indications
- Mild to moderate neck pain
- Early-stage muscular strain
- Patients who cannot tolerate NSAIDs
Contraindications
- Chronic liver disease
- Alcohol dependence
- Overdose risk with prolonged high doses

3. Muscle Relaxants
Mechanism of Action
- Reduce excessive motor neuron firing
- Break the pain–spasm–pain cycle
Indications
- Acute torticollis
- Muscle spasm–dominant neck pain
- Postural overload syndromes
Contraindications
- Elderly patients (risk of drowsiness, falls)
- Severe liver impairment
- Long-term use (dependency risk)

4. Neuropathic Pain Medications
Mechanism of Action
- Modulate calcium channels and neurotransmitter release
- Reduce abnormal nerve firing
Indications
- Cervical radiculopathy
- Burning, tingling, electric-shock–type pain
- Disc bulge with nerve root irritation
Contraindications
- Severe kidney dysfunction (dose adjustment required)
- Excessive sedation risk
- Pregnancy (case-dependent)

5. Short-Term Oral Steroids
Mechanism of Action
- Potent anti-inflammatory action
- Reduce nerve root edema and chemical irritation
Indications
- Acute cervical disc prolapse
- Severe nerve compression pain
- Acute inflammatory flare-ups
Contraindications
- Diabetes mellitus (raises blood sugar)
- Active infection
- Osteoporosis with repeated use

6. Topical Analgesics
Mechanism of Action
- Local counter-irritation
- Superficial pain receptor modulation
Indications
- Mild muscular neck pain
- Patients intolerant to oral medications
Contraindications
- Open wounds or skin infections
- Severe deep structural pain

7. Antidepressants (Low Dose)
Mechanism of Action
- Enhance descending inhibitory pain pathways
- Improve sleep and pain threshold
Indications
- Chronic neck pain
- Central sensitization
- Poor sleep with pain
Contraindications
- Cardiac conduction abnormalities
- Drug interactions
- Not first-line for acute pain
8. Supplements (Vitamin D, B12, Magnesium)
Mechanism of Action
- Improve nerve conduction
- Support muscle and bone health
Indications
- Deficiency-related pain
- Neuromuscular fatigue
Contraindications
- Excess supplementation without testing
II. Interventional Pain Management Procedures
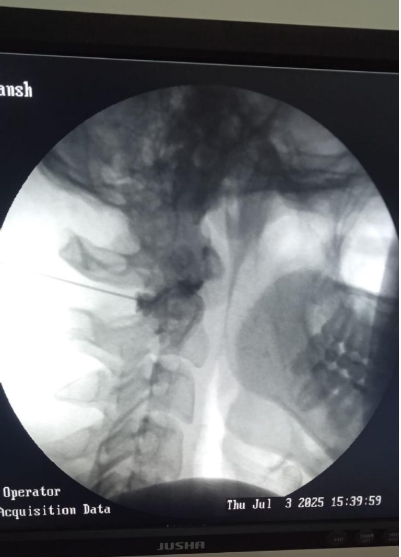
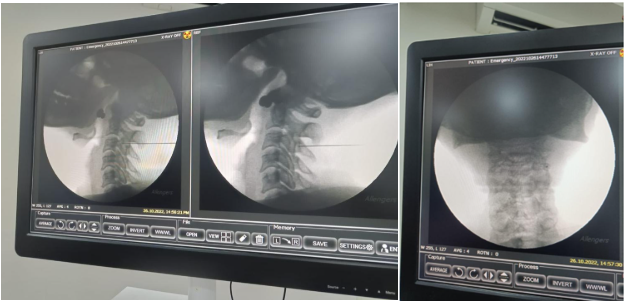
Fluoroscopy guided Intrartcular C1-C2 cervical facet joint anti inflammatory injection at Alleviate Pain Clinic, Bengaluru. Image Courtesy- Alleviate Pain Clinic
1. Cervical Facet Joint Injection
Mechanism of Action
- Steroid reduces inflammation inside the facet joint
- Local anesthetic breaks pain signaling
Indications
- Facet joint arthritis
- Neck pain worsened by extension or rotation
- Localized unilateral neck pain
Contraindications
- Active infection
- Bleeding disorders
- Unclear diagnosis
2. Cervical Medial Branch Block
Mechanism of Action
- Temporarily numbs sensory nerves supplying facet joints
- Confirms facet-mediated pain source
Indications
- Diagnostic confirmation before RFA
- Chronic mechanical neck pain
Contraindications
- Infection at injection site
- Severe spinal deformity without imaging guidance
3. Radiofrequency Ablation (RFA)
Mechanism of Action
- Controlled heat lesion deactivates pain-transmitting nerves
- Does not affect muscle strength or movement
Indications
- Chronic facet joint pain
- Positive response to medial branch blocks
- Pain > 3–6 months
Contraindications
- Uncertain diagnosis
- Acute inflammatory pain
- Pregnancy (relative)
4. Cervical Epidural Steroid Injection
Mechanism of Action
- Reduces nerve root inflammation
- Improves nerve mobility
Indications
- Cervical disc bulge or prolapse
- Arm pain, numbness, tingling
- MRI-confirmed nerve compression
Contraindications
- Active infection
- Bleeding disorders
- Uncontrolled diabetes
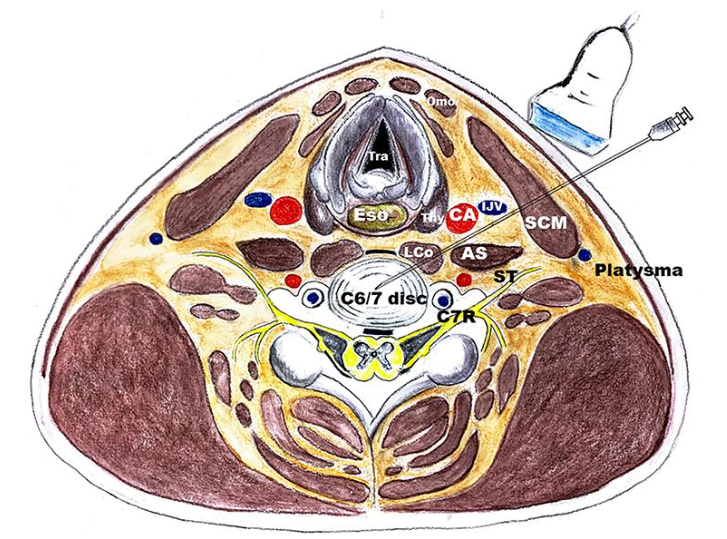
5. Ultrasound-Guided Trigger Point Injections
Mechanism of Action
- Deactivates taut muscle bands
- Restores muscle length and circulation
Indications
- Myofascial pain syndrome
- Postural neck pain
- Office-related neck pain
Contraindications
- Bleeding disorders
- Needle phobia (relative)
III. Regenerative Medicine Procedures

1. Platelet-Rich Plasma (PRP)
Mechanism of Action
- Delivers concentrated growth factors
- Stimulates tissue repair and collagen regeneration
Indications
- Cervical ligament laxity
- Early degenerative facet disease
- Chronic neck pain not responding to injections
Contraindications
- Active infection
- Platelet disorders
- Blood cancers
2. Prolotherapy
Mechanism of Action
- Mild inflammatory stimulus triggers ligament healing
- Improves joint stability
Indications
- Cervical instability
- Recurrent neck pain with normal MRI
- Post-whiplash pain
Contraindications
- Autoimmune flare-ups
- Uncontrolled diabetes
- Acute infection
IV. Multidisciplinary Approach at Alleviate Pain Clinic
Why medicines or injections alone are not enough
At Alleviate, treatment integrates:
- Pain physician–led diagnosis
- Imaging correlation
- Precision injections
- Regenerative repair
- Physiotherapy & posture correction
- Ergonomic and lifestyle counseling
This prevents recurrence and dependency on medicines.
When to Escalate Beyond Medicines
- Pain lasting > 4–6 weeks
- Recurrent episodes
- Pain radiating to arms
- Dependence on painkillers
- Structural abnormalities on imaging
Conclusion
Medicines provide symptom relief—but lasting recovery from neck pain requires targeting the anatomical and biological source of pain.
At Alleviate Pain Clinic, we combine mechanism-driven medicines, image-guided interventional pain management, regenerative therapies, and rehabilitation to deliver durable, non-surgical outcomes.
Frequently Asked Questions (FAQs)
There is no single best medicine for neck pain because treatment depends on the pain generator. Paracetamol suits mild muscular pain, NSAIDs help inflammatory causes, muscle relaxants relieve spasms, and neuropathic agents treat nerve pain. A mechanism-based medical evaluation ensures the most effective and safest medicine choice.
For fast relief, combine short-term medicines for neck pain (paracetamol or NSAIDs), local heat therapy, gentle stretching, and posture correction. If pain radiates to the arm or persists beyond a few weeks, image-guided injections such as trigger point injections or epidural steroids may provide quicker, targeted relief.
Effective natural neck pain remedies include warm compresses, ergonomic correction, regular neck mobility exercises, magnesium-rich nutrition, and adequate sleep support. Mind–body techniques like yoga and breathing exercises help reduce muscle tension. However, persistent or radiating pain should be medically evaluated to rule out structural causes.
Neck pain commonly arises from muscle strain, poor posture, cervical facet joint irritation, disc bulge, or nerve root compression. Modern lifestyle factors prolonged screen use, forward head posture, and stress are major contributors. Identifying the exact anatomical pain generator is essential for selecting the correct treatment approach.
The best treatment depends on the cause. Acute muscular pain responds to medicines and physiotherapy, while chronic facet pain may require medial branch blocks or radiofrequency ablation. Disc-related nerve pain often benefits from epidural injections. A multidisciplinary, image-guided, mechanism-based plan provides the most durable neck pain relief.
Take neck pain medicines strictly as prescribed. Paracetamol and NSAIDs are usually taken after food to reduce gastric irritation. Muscle relaxants are often given at night due to drowsiness. Avoid self-medication, dose escalation, or prolonged use without medical supervision, especially if you have liver, kidney, or gastric issues.
Neck pain medicines work through different mechanisms. Paracetamol alters central pain perception, NSAIDs reduce inflammatory prostaglandins, muscle relaxants break the pain–spasm cycle, and neuropathic agents stabilize abnormal nerve firing. Proper drug selection targets the underlying pain pathway rather than merely masking symptoms.
Timing depends on the drug class. NSAIDs and paracetamol are typically taken after meals, muscle relaxants are often preferred at night, and neuropathic medicines are usually given in the evening to minimize daytime sedation. Always follow your physician’s schedule for optimal efficacy and safety.