Chest pain in women is common, complex, and often misunderstood. While many people immediately associate chest pain with heart disease, the reality – especially for women – is far more nuanced. Women experience chest pain differently than men, and the causes range from cardiac and gastrointestinal issues to musculoskeletal and psychological factors.
Understanding these differences is crucial for early diagnosis, appropriate treatment, and prevention of serious complications.
At Alleviate Pain Clinic, we frequently see women who have undergone multiple tests yet continue to suffer from unexplained or recurring chest pain. This blog breaks down the complete picture, helping you understand the causes, warning signs, and when to seek medical attention.
Why Do Women Experience Chest Pain Differently Than Men?
Women often present with atypical symptoms compared to men. Instead of classic crushing chest pain, women may experience:
- Burning or tightness rather than pressure
- Pain radiating to the neck, jaw, shoulder blades, or upper back
- Nausea, fatigue, dizziness, or shortness of breath
- Chest discomfort associated with stress or exertion
Hormonal influences, smaller coronary vessels, differences in pain perception, and higher rates of non-cardiac causes all contribute to these variations. As a result, chest pain in women is sometimes misattributed to anxiety or acidity, delaying diagnosis.
Common Causes of Chest Pain in Women
Chest pain can arise from multiple systems in the body. Understanding these categories helps guide appropriate evaluation and care.
Heart-Related Causes of Chest Pain
1. Angina
Angina occurs when the heart muscle does not receive enough oxygen-rich blood. In women, it may present as:
- Chest tightness or burning
- Shortness of breath
- Fatigue or weakness rather than severe pain
It often worsens with exertion or emotional stress and improves with rest.
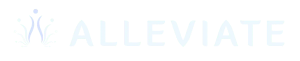
2. Heart Attack
Heart attacks in women may not always involve severe chest pain. Symptoms can include:
- Pressure, squeezing, or discomfort in the chest
- Pain in the jaw, neck, upper back, or arms
- Nausea, sweating, lightheadedness
- Extreme fatigue
These subtle symptoms make early recognition critical.
3. Coronary Artery Disease (CAD)
CAD involves narrowing or blockage of coronary arteries. Women may develop microvascular disease, affecting smaller vessels, which can cause chest pain even when angiograms appear normal.
4. Aortic Dissection
A rare but life-threatening condition where the inner layer of the aorta tears. Pain is typically:
- Sudden and severe
- Tearing or ripping in nature
- Radiating to the back
Immediate emergency care is essential.
Digestive Causes of Chest Pain
1. Gastroesophageal Reflux Disease (GERD)
One of the most common non-cardiac causes of chest pain. Symptoms include:
- Burning sensation behind the breastbone
- Pain after meals or when lying down
- Sour taste or regurgitation
GERD-related pain can closely mimic heart pain.
2. Esophageal Spasms
Sudden, involuntary contractions of the esophagus can cause:
- Intense chest pain
- Difficulty swallowing
- Pain triggered by hot or cold foods
3. Gallbladder or Pancreas Issues
Gallstones or pancreatitis can cause pain that:
- Radiates to the chest or back
- Occurs after fatty meals
- Is associated with nausea or vomiting
Lung-Related Causes of Chest Pain
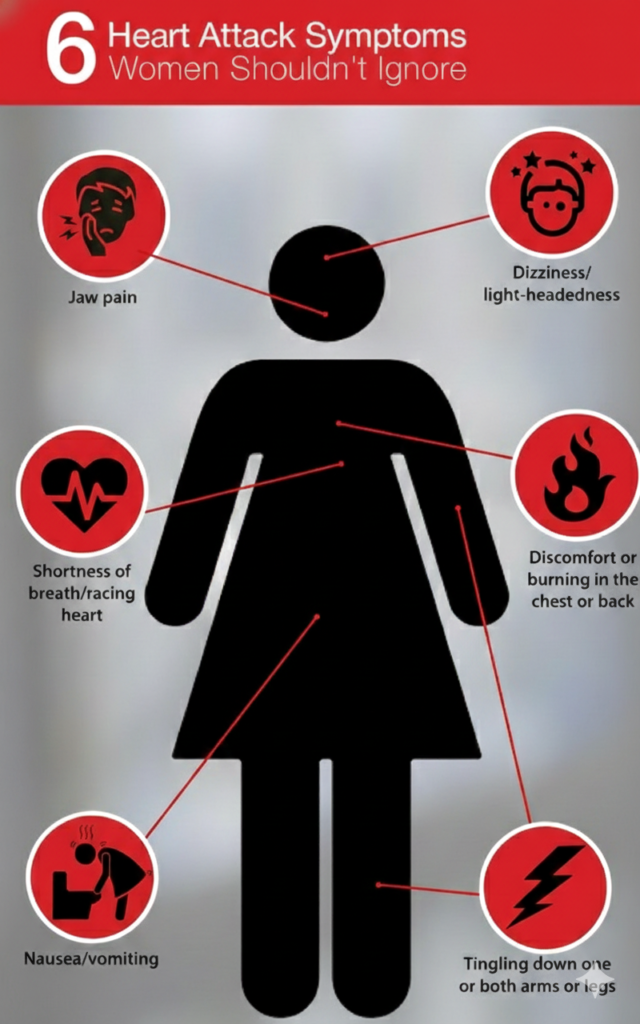
1. Pulmonary Embolism
A blood clot in the lungs causing:
- Sudden sharp chest pain
- Shortness of breath
- Rapid heart rateThis is a medical emergency.
2. Pleurisy
Inflammation of the lung lining leading to:
- Sharp pain during breathing or coughing
- Pain relieved by shallow breathing
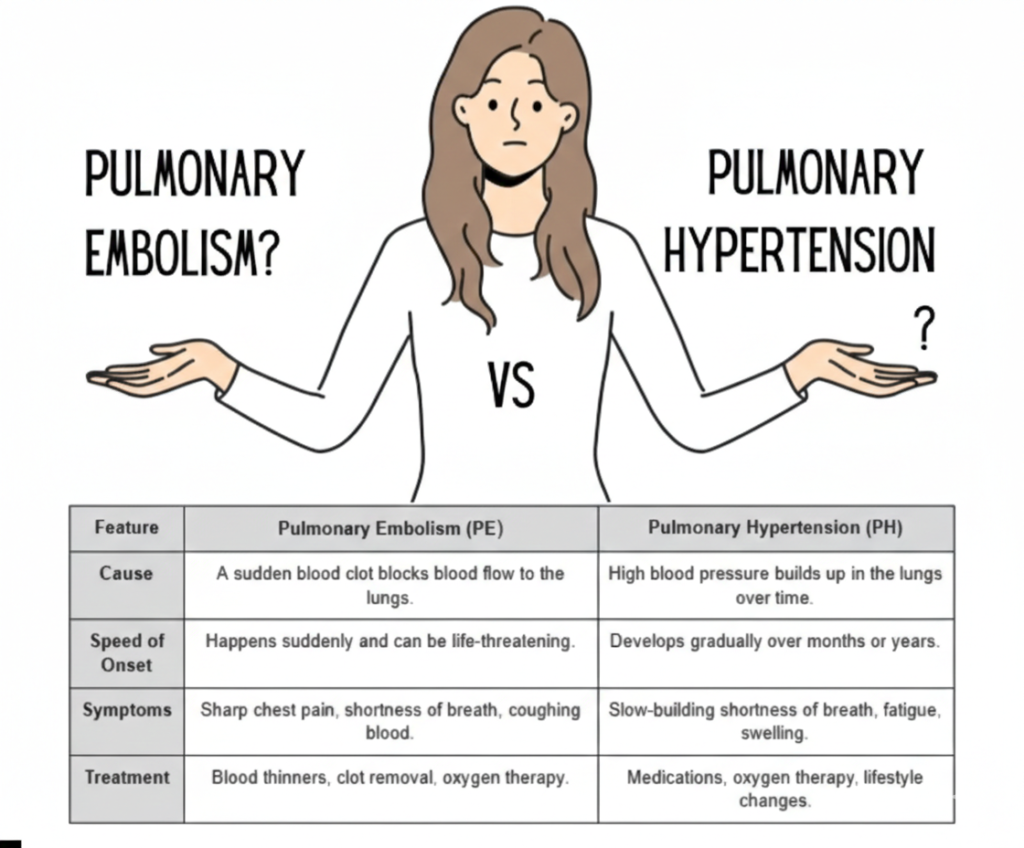
3. Pneumonia
Chest pain may occur due to infection-related inflammation, often accompanied by:
- Fever
- Cough
- Breathlessness
4. Collapsed Lung (Pneumothorax)
Sudden onset of chest pain with difficulty breathing, more common in smokers or after trauma.
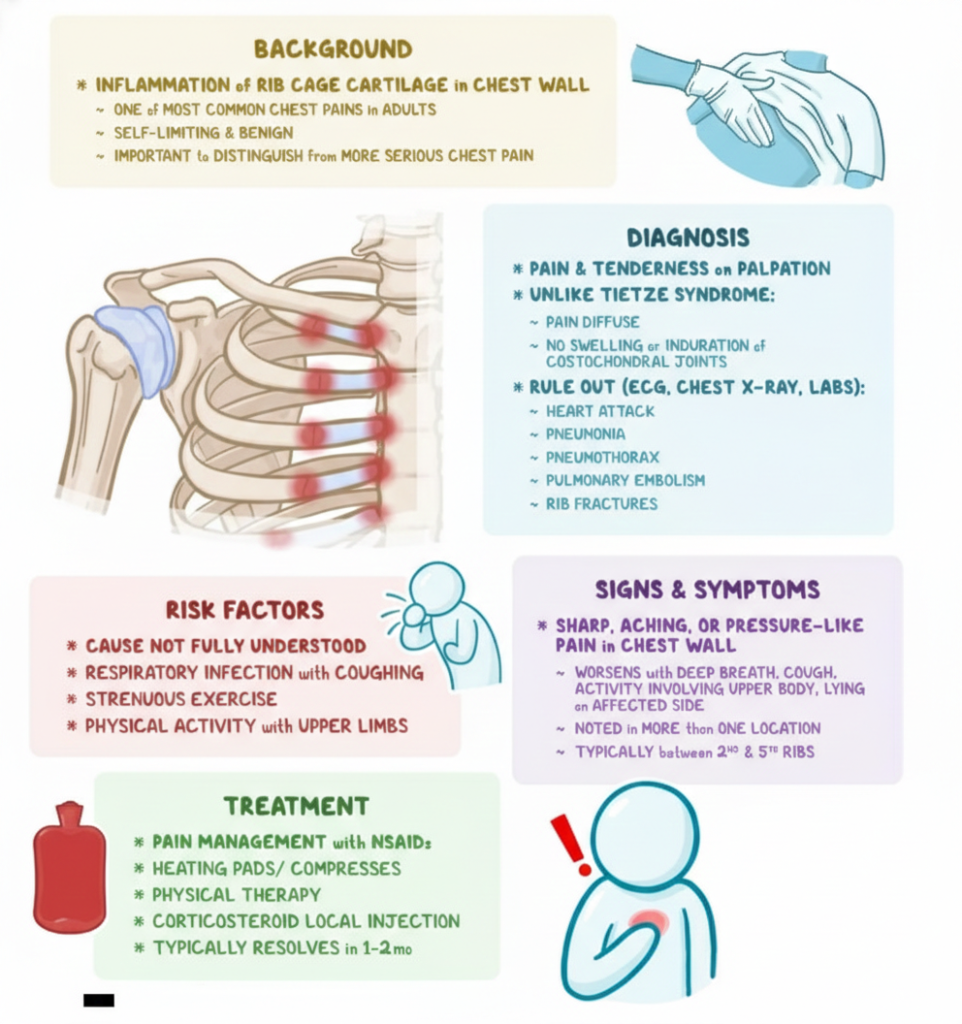
Musculoskeletal Causes of Chest Pain
Musculoskeletal causes are very common, especially in women.
These include:
- Costochondritis (inflammation of rib cartilage)
- Muscle strain from posture, lifting, or exercise
- Cervical or thoracic spine dysfunction
- Myofascial trigger points
Pain often:
- Worsens with movement or touch
- Improves with rest or posture correction
Psychological Causes of Chest Pain
Musculoskeletal causes are very common, especially in women.
These include:
- Costochondritis (inflammation of rib cartilage)
- Muscle strain from posture, lifting, or exercise
- Cervical or thoracic spine dysfunction
- Myofascial trigger points
Pain often:
- Worsens with movement or touch
- Improves with rest or posture correction
Psychological Causes of Chest Pain
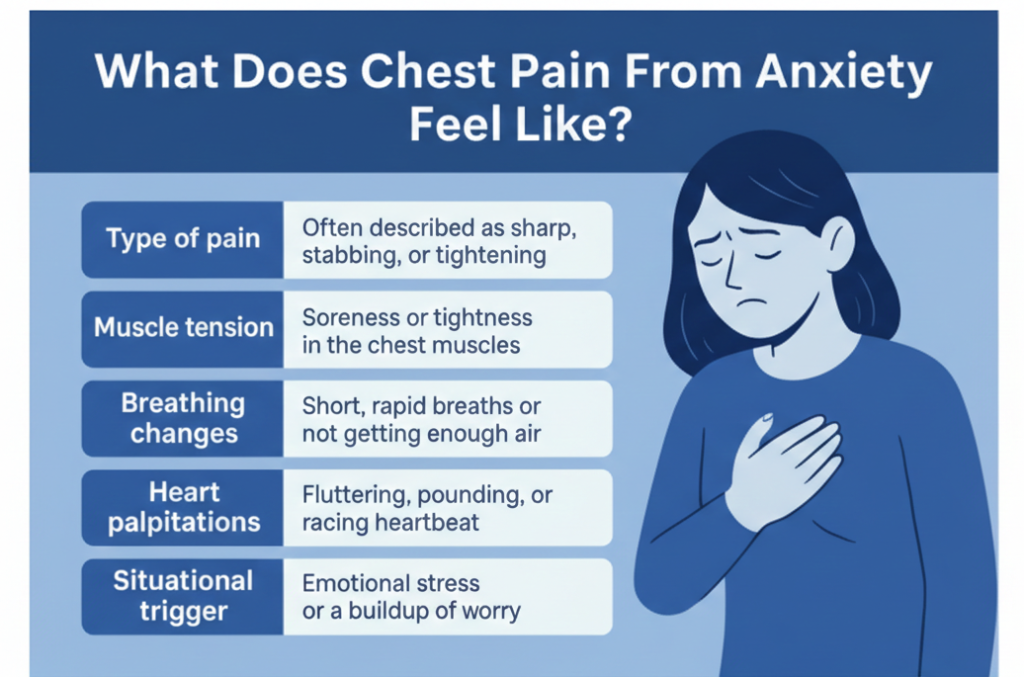
1. Anxiety and Panic Attacks
Chest pain associated with anxiety may feel intense and frightening. Common features:
- Tightness or sharp pain
- Rapid breathing
- Palpitations
- Sense of impending doom
Though not life-threatening, symptoms can closely resemble a heart attack.
2. Chronic Stress
Long-term stress can cause:
- Persistent chest tightness
- Muscle tension
- Autonomic nervous system imbalance
Stress also increases the risk of heart disease, creating a dual impact.
Understanding Chest Pain by Location
Left-Sided Chest Pain in Women
Often raises concern for heart-related issues but can also arise from:
- GERD
- Muscular strain
- Anxiety
Always warrants medical evaluation.
Right-Sided Chest Pain in Women
More commonly linked to:
- Gallbladder disease
- Lung conditions
- Musculoskeletal causes
Central Chest Pain
Can be associated with:
- Angina
- GERD
- Anxiety or panic attacks
When Should You See a Doctor?
Seek immediate medical care if chest pain is:
- Sudden, severe, or worsening
- Associated with breathlessness, sweating, fainting
- Radiating to jaw, arm, or back
- Occurring with known heart risk factors
Do not self-diagnose chest pain.
Risk Factors for Chest Pain in Women
- High blood pressure
- Diabetes
- Smoking
- Obesity
- Sedentary lifestyle
- Chronic stress
- Hormonal changes (menopause)
- Family history of heart disease
Prevention and Management Strategies
- Regular health check-ups
- Heart-healthy diet and exercise
- Stress management and sleep optimisation
- Posture correction and musculoskeletal care
- Early evaluation of recurring symptoms
Alleviate Pain Clinic’s Multidisciplinary Approach
At Alleviate Pain Clinic, we understand that chest pain in women often has multiple overlapping causes.
Our approach includes:
- Detailed clinical evaluation to rule out cardiac emergencies
- Assessment of musculoskeletal, nerve, and spinal contributors
- Management of chronic pain syndromes and stress-related pain
- Collaboration with cardiology, pulmonology, and gastroenterology when needed
- Individualised treatment plans focused on long-term relief, not just symptom suppression
Warning Signs You Should Never Ignore
- New-onset chest pain after 40
- Chest pain with exertion
- Pain associated with breathlessness or fainting
- Persistent or recurrent chest discomfort
Conclusion
Chest pain in women is not one-size-fits-all. It can arise from the heart, lungs, digestive system, muscles, or mind—and often from a combination of these. Understanding the complete picture empowers women to seek timely care and avoid unnecessary suffering.
If you or someone you love is experiencing chest pain that is unexplained, recurring, or worrying, early evaluation can be lifesaving.
Book a consultation at Alleviate Pain Clinic to receive a comprehensive, multidisciplinary assessment and a personalised care plan focused on clarity, safety, and lasting relief.
Frequently Asked Questions (FAQs)
Chest pain in women can arise from the heart, lungs, digestive system, muscles, or stress-related causes. Women often experience atypical symptoms, such as burning, tightness, or fatigue rather than classic pressure. Because causes vary widely from GERD to angina, persistent, severe, or unexplained chest pain should always be medically evaluated promptly.
Yes. Gas and acid reflux (GERD) can cause left-sided chest pain in women, often described as burning behind the breastbone, bloating, or discomfort after meals. However, because left-sided pain can also signal heart disease, any new, severe, or persistent symptoms should be assessed to safely rule out cardiac causes.
Common cardiac causes include angina, coronary artery disease (including microvascular disease), and heart attack. Women may experience atypical symptoms such as fatigue, shortness of breath, nausea, or back and jaw pain. Risk factors like diabetes, hypertension, smoking, and menopause significantly increase the likelihood of heart-related chest pain.
Anxiety and chronic stress activate the autonomic nervous system, causing rapid breathing, muscle tension, and chest wall tightness that can mimic heart pain. Panic attacks may produce sharp or pressure-like discomfort. While often benign, recurrent symptoms should still be evaluated to exclude cardiac, pulmonary, or gastrointestinal causes.
Central chest pain can result from angina, GERD, esophageal spasm, anxiety, or costochondritis. Cardiac causes typically worsen with exertion, while reflux-related pain often follows meals or lying down. Because symptoms can overlap significantly, persistent, severe, or unexplained central chest pain requires proper medical assessment for accurate diagnosis.