Trigeminal neuralgia (TN) is defined by recurrent unilateral brief
Trigeminal neuralgia (TN) is defined by recurrent unilateral brief electric shock-like pain in the distribution of the trigeminal nerve, which is abrupt in its onset and termination. The pain is restricted to one or more of the trigeminal divisions and is triggered by innocuous sensory stimuli. TN is divided into either classical TN (CTN) or secondary TN (STN) caused by multiple sclerosis or a space-occupying lesion such as a tumor, cerebral aneurism or a megadolicho basilar artery.
Epidemiology
TN is frequently both misdiagnosed and underdiagnosed. The incidence of TN is variably reported between studies, with a range from 4.3 to 27 new cases per 100,000 people per year (2–4). The incidence is higher among women, and increases with age (2). The lifetime prevalence was estimated to be 0.16–0.3% in population-based studies (3,5). The average age of onset is 53 years in classical TN and 43 years in secondary TN, but the age of onset can range from early to old age (1,6). In tertiary care-based studies, STN accounted for 14–20% of TN patients (1,7).
Etiology and Pathogenesis
Dandy proposed as early as 1930 that conservatively speaking the cause behind 30% of the patients afflicted with Trigeminal Neuralgia was due to compression of the trigeminal nerve by a blood vessel.[8] As of today the consensus behind the etiology of Classical Trigeminal Neuralgia is either compression or morphological changes in the trigeminal nerve brought about usually an artery in the cerebellopontine cistern. This is termed as ‘NEUROVASCULAR CONFLICT’ with compression. Transition of Schwann cell myelination to oligodendroglia myelination was observed in many anatomical specimens. [9]
Evidence in recent times is in favour of a neuromuscular conflict characterised by
neurovascular conflict involving morphological changes of distortion, distension, indendation,dislocation , flattening or atrophy of the trigeminal nerve is a hallmark feature of upto half the patients suffering from Classical Trigeminal Neuralgia.[10-12] Conversely, there is a line of thought whether ‘simple contact’ between structures might play a role in the etiology.[10-12]
Figure 1. MRI in a patient with left-sided classical trigeminal neuralgia. Balanced fast field echo sequence of the fossa posterior, axial plane, at the level of the pons. The left trigeminal nerve (right-sided arrowhead) is displaced by an arterial loop (arrows) from the anterior inferior cerebellar artery.
Various studies point towards focal demyelination of primary trigeminal afferents adjacent to the entry of the root of the trigeminal nerve into the pons, as the chief underlying pathophysiology in people suffering with Trigeminal Neuralgia.[13-15]
In Secondary TN, though the pathophysiological mechanism is the same as Classical TN, the etiology is governed by different structural lesions such as plaques of Multiple Sclerosis affecting the trigeminal root or a space-occupying lesion in the cerebellopontine cistern such as epidermoid tumours, meningiomas, neurinomas, arteriovenous malformations or aneurysms (shown in figure below) (16,17)).
Figure showing MRI in a patient with left-sided symptomatic trigeminal neuralgia. Balanced fast field echo sequence of the fossa posterior, axial plane at the level of the pons. The peripheral part of the left trigeminal nerve is displaced by a meningioma (both structures encircled).
SYMPTOM COMPLEX OF Trigeminal Neuralgia
The original term coined for this condition was Tic Doloureux[18], keeping in mind the characteristic wince seen in TN patients at the time of a pain paroxysm.
The pain has been described by patients as being of a sharp, shooting and stabbing in nature and mimicking electric shock- like sensations. The pain paroxysm of Trigeminal Neuralgia is an extremely painful and debilitating experience for the system. The sudden and unexpected onset makes this highly unpleasant pain even more horrifying for patients.
A Pain Paroxysm can last from a fraction of a second to several times a day because these paroxysms are sometimes set into continuous recurrence following a refractory period. This may be experienced as a series of attacks with many paroxysms punctuating close together. The paroxysmal pain may be accompanied by a continuous pain of a dull achy nature in the background and milder in intensity. [19-21]This background headache has been observed more commonly in women.[19,22,23]
- Refractory period and trigger factors
Patients usually experience a refractory period following the paroxysmal attack where another attack cannot be triggered. Hyperpolarisation of the sensory neuron has been deemed responsible for this phenomena.[24]Many patients experience a refractory period after a paroxysmal attack where new attacks cannot be elicited. The pathophysiological mechanism of this phenomenon is unknown. It has been proposed that it is caused by hyperpolarisation of the sensory neuron (24).Kugelberg and lindbom, in their studies have drawn a direct relationship between the presence and duration of refractory period to the intensity and duration of the concluded attack.[25]
The pain of Trigeminal Neuralgia may be triggered by innocuous sensory stimuli to the side of the face. The stimuli might be intramural or extra oral. The commonly seen triggers include normal daily activities such as light touch, talking, chewing, brushing teeth and cold wind against the face (26,27)
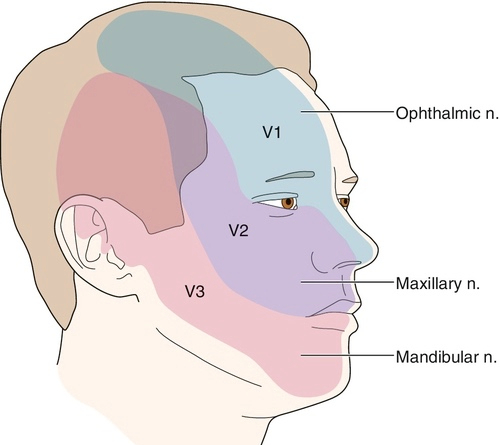
- Site of lesion
The second or third division of the trigeminal nerve is most commonly affected. Right side is affected more often. (11)Bilateral TN is rare in the classical form and should be indicative of a case of Secondary TN.
FIGURE 117.1 Dermatomes for trigeminal nerve. V1, ophthalmic nerve. V2, maxillary nerve. V3, mandibular nerve. (From Waldman SD. Trigeminal nerve block: coronoid approach. In Waldman SD, ed. Atlas of Interventional Pain Management, 2nd ed. Philadelphia, WB Saunders, 2004
- Natural Progression
It was earlier strongly believed that the pain of TN worsens over time and becomes chronic characterised There are very few studies examining the natural history of TN. It has been proposed that pain may worsen with time and that TN in its chronic state is characterised by longer lasting, medically refractory pain, sensory disturbances and progressive neuroanatomical changes of the trigeminal root (23). In recent times, studies have challenged this belief by showing that in majority of patients, the pain did not increase in frequency or duration, nor did it become refractory to medication and even the dosage threshold remained more or less constant.[] Another common observation is periods of complete remission lasting for months and in some cases even years. This can be attributed to reduction in nerve excitability and partial demyelination.[24]
- Facial pain associated with autonomic features
Tearing and rhinorrhea have been long associated with TN . Autonomic symptoms are part of the symptom complex in a majority of TN patients. [26,27,29] This is believed to be the result of the trigeminovascular reflex which tends to get elicited by intense facial pain.[30] The differential diagnosis include short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT), and short-lasting unilateral neuralgiform headache attacks with autonomic symptoms (SUNA) (31).
DIAGNOSIS- The diagnosis of TN is essentially based on the history . The onset of pain is a very important component of the history taking . History of any preceding Herpes Zoster rash in the affected area, any invasive dental procedures or significant trauma to the ipsilateral side of the face is a must. A dental procedure or trauma can point towards Post Traumatic Trigeminal Neuropathy(PPTN). PPTN may be comparable to TN but it is marked by clear cut sensory abnormalities.[29]
A thorough dental check up is warranted to rule out a cracked tooth(probably due to chewing hard foods), which might present like the pain of TN. Bilateral constant pain in the jaw area might raise the possibility of tension-type headache, temporomandibular joint disorder and persistent idiopathic facial pain.
Other differential diagnosis include Occipital neuralgia, paroxysmal hemicrania, glossopharyngeal neuralgia , short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT), and short-lasting unilateral neuralgiform headache attacks with autonomic symptoms (SUNA)
Though primarily a clinical diagnosis, Magnetic resonance imaging (MRI) imaging can detect changes in trigeminal root, any neuromuscular compression and to rule out secondary pathology. MRI can diagnose entire course of nerve,[32] root atrophy, and CPA cistern.
3D fast imaging employing steady-state acquisition(FIESTA)[33,34] and contrast-enhanced 3D time-of-flight (TOF) magnetic resonance angiography (MRA) in combination with unenhanced MRA are becoming popular in detecting the vessel involved and in detecting the vascular conflict.
Treatment
Abortive treatments haven’t been successful for managing Trigeminal Neuralgia but the mainstay remains pharmacological management. Ablative and non ablative interventional procedures are reserved for patients for medical management fails to control the symptoms.
Carbamazepine and oxcarbazepine
The first- line management offered to patients suffering with TN are Carbamazepine and oxcarbazepine. They are seen to be effective in delivering initial pain control in upto 90% of the patients [35] although the effects may unfortunately wane down with chronicity. The potent side effect profile of these drugs leads to withdrawal of their use in upto 40% of the patients.[36] Women are less tolerant to these medications. Carbamazepine use in patients with other significant comorbidities is difficult as it tends to have interactions with other medications. Oxcarbazepine, though causes fewer side effects, can bring about central nervous system depression or dose related hyponatremia.( decreased sodium)
Clinical response to both drugs differs in patients considerably. One can be replaced with the other to get a better response. ‘200 mg of carbamazepine is equipotent to 300 mg of oxcarbazepine’. While the effects of these drugs are significant in the control of paroxysmal pain
Lamotrigine
Lamotrigine is generally recommended as an add-on therapy for patients showing poor tolerance to carbamazepine and oxcarbezepine. It is generally associated with fewer side effects than carbamazepine and oxcarbazepine
Gabapentin and pregabalin
Clinical application has shown gabapentin and pregabalin to be less effective but having fewer side effects than carbamazepine and oxcarbazepine. They can therefore be used in place of or in addition to carbamazepine or oxcarbazepine. However, they do pose a risk of dependency.
Baclofen
Baclofen is particularly helpful in patients with a background of Multiple Sclerosis where it might be used for managing spasticity.
Botulinum toxin type A
Recent studies focussing on the efficacy of subcutaneous injection and injection over the gingival mucosa (of Botulin Toxin Type A) , found significant improvement in symptoms as compared to placebo. Transient facial edema and and transient facial weakness were some of the mild side effects.
Acute treatment for severe exacerbation
Severe exacerbations ,which are marked by intense painful episodes with increasing frequency and difficulty in even eating or drinking are managed by hospital admission for immediate rehydration, maintenance of nutrition, short-term pain management and long-term optimisation of preventive treatments. Opiods are often used during such episodes but their efficacy has been questioned. Local anaesthetic injections or topical lidocaine can be effective for instantly reducing the pain from trigger zones. Intravenous infusions of fosphenytoin (15 mg/kg over 30 min) and lidocaine (5 mg/kg over 60 min) under cardiac monitoring can be highly effective.
Non Surgical Interventional treatments:-
These are considered for debilitating pain refractory to medicines. They can be divided into
- Needle based Controlled Radiofrequency lesioning of the trigeminal ganglion.
- Mechanical ballon compression of the trigeminal ganglion.
- Glycerol based chemical rhizolysis
- Internal Neurolysis- Separation of the trigeminal nerve fascicles in the posterior fossa.
- Stereotactic Radiosurgery focussing radiation at the trigeminal root entry zone.
At ALLEVIATE for patients not responding to medical management the treatment of choice is, Image guided Controlled Radiofrequency Lesioning of the Trigeminal Ganglion.
Surgical intervention for trigeminal neuralgia
Patients not responding to any of the above stated treatment modalities are faced with the surgical option of Microvascular decompression. Surgeon has to be really careful due to the proximity of neurovascular structures to the operating field.Microvascular decompression has better results in elderly with fewer co-morbidities as opposed to the younger population.
REFERENCES:-
- Maarbjerg, S, Gozalov, A, Olesen, J. Trigeminal neuralgia – a prospective systematic study of clinical characteristics in 158 patients. Headache 2014; 54: 1574–1582
- Katusic, S, Beard, CM, Bergstralh, E. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945–1984. Ann Neurol 1991; 27: 89–95.
- Mueller, D, Obermann, M, Yoon, MS. Prevalence of trigeminal neuralgia and persistent idiopathic facial pain: A population-based study. Cephalalgia 2011; 31: 1542–1548.
- MacDonald, BK, Cockerell, OC, Sander, JW. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain 2000; 123: 665–676.
- Sjaastad, O, Bakketeig, LS. The rare, unilateral headaches. Vågå study of headache epidemiology. J Headache Pain 2007; 8: 19–27.
- De Simone, R, Marano, E, Brescia Morra, V. A clinical comparison of trigeminal neuralgic pain in patients with and without underlying multiple sclerosis. Neurol Sci 2005; 26: 150–151.
- Cruccu, G, Biasiotta, A, Galeotti, F. Diagnostic accuracy of trigeminal reflex testing in trigeminal neuralgia. Neurology 2006; 66: 139–41.
- Dandy, WE . Concerning the cause of trigeminal neuralgia. Am J Surg 1934; 24: 447–455.
- Peker, S, Kurtkaya, O, Uzun, I. Microanatomy of the central myelin-peripheral myelin transition zone of the trigeminal nerve. Neurosurgery 2006; 59: 354–359.
- Maarbjerg, S, Wolfram, F, Gozalov, A. Significance of neurovascular contact in classical trigeminal neuralgia. Brain 2014; 138: 311–319.
- Antonini, G, Di Pasquale, A, Cruccu, G. MRI contribution for diagnosing symptomatic neurovascular contact in classic trigeminal neuralgia. A blinded case-control study and meta-analysis. Pain 2014; 155: 1464–1471.
- Masur, H, Papke, K, Bongartz, G. The significance of three-dimensional MR-defined neurovascular compression for the pathogenesis of trigeminal neuralgia. J Neurol 1995; 242: 93–98.
- Rappaport, ZH, Govrin-Lippmann, R, Devor, M. An electron-microscopic analysis of biopsy samples of the trigeminal root taken during microvascular decompressive surgery. Stereotact Funct Neurosurg 1997; 68: 182–186.
- Lutz, J, Thon, N, Stahl, R. Microstructural alterations in trigeminal neuralgia determined by diffusion tensor imaging are independent of symptom duration, severity, and type of neurovascular conflict. J Neurosurg 2015; 124: 823–830.
- Obermann, M, Yoon, M-S, Ese, D. Impaired trigeminal nociceptive processing in patients with trigeminal neuralgia. Neurology 2007; 69: 835–841.
- Nomura T, Ikezaki K, Matsushima T et al. Trigeminal neuralgia: Differentiation between intracranial mass lesions and ordinary vascular compression as causative lesions. Neurosurg Rev 1994; 17: 51–57.
- Jensen, TS, Rasmussen, P, Reske-Nielsen, E. Association of trigeminal neuralgia with multiple sclerosis: Clinical and pathological features. Acta Neurol Scand 1982; 65: 182–189.
- Cole, CD, Liu, JK, Apfelbaum, RI. Historical perspectives on the diagnosis and treatment of trigeminal neuralgia. Neurosurg Focus 2005; 18: 1–15.
Google Scholar | Crossref
- Maarbjerg, S, Gozalov, A, Olesen, J. Concomitant persistent pain in classical trigeminal neuralgia – evidence for different subtypes. Headache 2014; 54: 1173–1183.
Google Scholar | Crossref | Medline | ISI
- Rasmussen, P . Facial pain. II. A prospective survey of 1052 patients with a view of: Character of the attacks, onset, course, and character of pain. Acta neurochir 1990; 107: 121–128.
Google Scholar | Crossref | Medline | ISI
- Brisman, R . Constant face pain in typical trigeminal neuralgia and response to gamma knife radiosurgery. Stereotact Funct Neurosurg 2013; 91: 122–128.
Google Scholar | Crossref | Medline | ISI
- Maarbjerg, S, Wolfram, F, Gozalov, A. Association between neurovascular contact and clinical characteristics in classical trigeminal neuralgia: A prospective clinical study using 3.0 Tesla MRI. Cephalagia 2015; 35: 1077–1084.
Google Scholar | SAGE Journals | ISI
- Burchiel, KJ, Slavin, KV. On the natural history of trigeminal neuralgia. Neurosurgery 2000; 46: 152–154.
Google Scholar | Crossref | Medline | ISI
- Devor, M, Amir, R, Rappaport, ZH. Pathophysiology of trigeminal neuralgia: The ignition hypothesis. Clin J Pain 2002; 18: 4–13
Google Scholar | Crossref | Medline | ISI
- Kugelberg, E, Lindblom, U. The mechanism of the pain in trigeminal neuralgia. J Neurol Neurosurg Psychiatry 1959; 22: 36–43.
Google Scholar | Crossref | Medline | ISI
- Maarbjerg, S, Gozalov, A, Olesen, J. Trigeminal neuralgia – a prospective systematic study of clinical characteristics in 158 patients. Headache 2014; 54: 1574–1582.
Google Scholar | Crossref | Medline | ISI
- Rasmussen, P . Facial pain. IV. A prospective study of 1052 patients with a view of: Precipitating factors, associated symptoms, objective psychiatric and neurological symptoms. Acta neurochir 1991; 108: 100–109. .
Google Scholar | Crossref | Medline | ISI
- Di Stefano, G, La Cesa, S, Truini, A. Natural history and outcome of 200 outpatients with classical trigeminal neuralgia treated with carbamazepine or oxcarbazepine in a tertiary centre for neuropathic pain. J Headache Pain 2014; 15: 1–5.
Google Scholar | Crossref | Medline | ISI
- Simms, HN, Honey, CR. The importance of autonomic symptoms in trigeminal neuralgia. Clinical article. J Neurosurg 2011; 115: 210–216.
Google Scholar | Crossref | Medline | ISI
- May, A, Goadsby, PJ. The trigeminovascular system in humans: Pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab 1999; 19: 115–127.
Google Scholar | SAGE Journals | ISI
- Cohen, AS, Matharu, MS, Goadsby, PJ. Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) or cranial autonomic features (SUNA) – a prospective clinical study of SUNCT and SUNA. Brain 2006; 129: 2746–2760.
Google Scholar | Crossref | Medline | ISI
- Cruccu, G, Gronseth, G, Alksne, J. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol 2008; 15: 1013–1028.
Google Scholar | Crossref | Medline | ISI
- Fertleman, CR, Baker, MD, Parker, KA. SCN9A mutations in paroxysmal extreme pain disorder: Allelic variants underlie distinct channel defects and phenotypes. Neuron 2006; 52: 767–774.
Google Scholar | Crossref | Medline | ISI
- Yang, Y, Wang, Y, Li, S. Mutations in SCN9A, encoding a sodium channel alpha subunit, in patients with primary erythermalgia. J Med Genet 2004; 41: 171–174.
Google Scholar | Crossref | Medline | ISI
- Cruccu G , Di Stefano G , Truini A . Trigeminal neuralgia. N Engl J Med2020;383:754–62.doi:10.1056/NEJMra1914484pmid:http://www.ncbi.nlm.nih.gov/pubmed/32813951
- O\’Callaghan L , Floden L , Vinikoor-Imler L , et al. Burden of illness of trigeminal neuralgia among patients managed in a specialist center in England. J Headache Pain2020;21:130. doi:10.1186/s10194-020-01198-z pmid: http://www.ncbi.nlm.nih.gov/pubmed/33167869