Achilles Tendonitis
TYPES:- Depending on the site of the tendon inflamed, Achilles Tendonitis can be classified into Insertional and Non Insertional tendonitis.
Noninsertional Achilles tendinitis Commonly seen in younger active individuals, the pathology is centred around the middle portion of the tendon exhibiting swelling, degeneration and tiny tears suggesting breakdown of the tendon fibres.
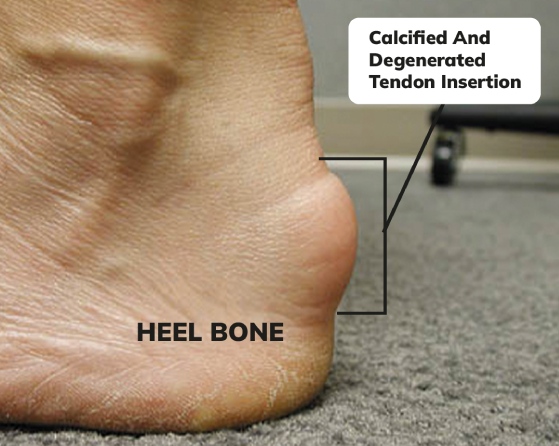
Insertional Achilles tendonitis Insertional Achilles tendonitis involves the attachment site of the tendon onto the heel bone. This is usually seen in older age groups resulting from years of overuse. Chronic cases of Insertional tendonitis are often associated with calcifications at the insertion.
CAUSES This condition usually results from repetitive stress on the Achilles tendon. Some common causes observed are :
- A sudden increase in the intensity of exercise without letting the body getting a chance to acclimtize to the increased workload.eg- sudden drastic increase in the distance one runs daily
- Tightness in the calf muscles – Having tight calf muscles and suddenly starting an aggressive exercise program can put extra stress on the Achilles tendon
Bone spur due to extra bone growth where the Achilles tendon attaches to the heel bone can irritate the tendon and cause pain.
HISTOPATHOLOGY:- The hallmark features of the tendon histopathology that are observed are cellular activation and increase in cell numbers, increase in ground substance, collagen disarray and neovascularisation. It is not considered to be a primarily inflammatory condition. Histological evaluation of biopsies shows intratendinous microdialysis[1,2],Neurogenic inflammation, though has been distinctly associated with this condition[3] Peptides released from peptidergic group IV fibres in response to peripheral noxious stimuli are responsible for the initiation of many pathophysiological processes. Moreover, neuropeptides such as substance P and calcitonin gene- related peptide point towards an inflammatory process in the tendon.
SYMPTOMS:- The usual symptoms of Achilles tendonitis include:
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Swelling that is present all the time and gets worse throughout the day with activity
A sudden pop at the back of the ankle might indicate partial or complete rupture of the Achilles tendon.
CLINICAL EXAMINATION:- Careful clinical examination of the foot and ankle in a case of Achilles Tendonitis can lead to some of these findings
- Swelling along the Achilles tendon or at the back of your heel
- Enlargement or thickening of the Achilles tendon
- Bony spurs at the lower part of the tendon at the back of your heel indicate insertional tendonitis
- The point of maximum tenderness
- Pain in the middle of the tendon point towards noninsertional tendonitis.
- Pain at the back of your heel at the lower part of the tendon is common in insertional tendonitis
- Limited range of motion in your ankle – specifically, a decreased ability to flex your foot
- A palpable gap may indicate towards a tendon rupture.
INVESTIGATION:- X – rays can provide information on any calcification at the insertion pointing towards Insertional Achilles Tendonitis. Sometimes in cases of chronic insertional tendonitis calcifications might be noticed along the middle portion of the tendon. Additionally x rays can show additional heel spurs.
MRI, though is not useful directly in the diagnosis, it is often used by surgeons for planning surgery for the diseased tendon.
Treatment
INITIAL CONSERVATIVE APPROACH
Rest – The first step is to reduce the strain on the tendon by eliminating or substituting high impact activities with low impact ones. Instead of running patients are advised to use elliptical cross trainers and static cycles. In very acute and painful cases no exertion is advised till the pain comes down.
Ice- Icing the Achilles tendon a few times a day for 10-15 minute periods can help get the pain and inflammation down.
Non-steroidal anti-inflammatory medications such as ibuprofen and naproxen help in managing the pain and swelling but are usually not advised for more than a week at a stretch.
Exercise and Physical Therapy- The following exercise can help to strengthen the calf muscles and reduce stress on the Achilles tendon.
Calf stretch
- Calf stretch
Keeping the back leg straight with the heel placed on the ground one should lean forward against a wall. The front leg has a bend in the knee . To stretch the gastrocnemius complex(calf muscles) and the Achilles tendon, hips have to be pushed towards the wall in a controlled manner. Position is to be held for 10 seconds before relaxing. Excercise should be repeated around 20 times for each foot and this should give the adequate stretch in the calf muscles.Physical - Eccentric Strengthening Protocol
Eccentric strengthening is defined as contraction of a muscle while it is getting longer. Eccentric strengthening is more helpful for non insertional tendonitis. Once initiated for a a couple of weeks under the supervision of a physical therapist, these exercises can be performed at home following that.
Heel drop
Bilateral heel drop – Stand at the edge of a stair, or a raised platform that is stable, with just the front half of your foot on the stair, heels are lifted off the ground and brought back down to the lowest point possible in a controlled manner. This is to be repeated at least 20 times. Care is to be taken during the bilateral heel drop to be balanced correctly before starting.
Single leg heel drop – This exercise is similar to the bilateral heel drop, except that all the weight is balanced on one leg.
Amongst other physical therapy modalities, Extracorporeal shockwave therapy(ESWT) has found some success. It produces high- energy shock wave impulses stimulating healing in the damaged tendon.
Supportive Shoes and Orthotics , that can offload the tendon or cushion the heel can be helpful.
INTERVENTIONAL NON INVASIVE APPROAC – Blind or Ultrasound guided Cortisone injections have been used to ease the pain utilising the potent anti inflammatory effect of cortisone. Inadvertent repeated injections of cortisone at the insertion site can cause weakening and rupture of the tendon.
REGENERATIVE APPROACH
AT ALLEVIATE, we use a comprehensive approach of Platelet Rich Plasma with prolotherapy to treat Achilles Tendonitis not responding to conservative means. Procedures are carried out under strict image guidance using a high definition Musculoskeletal Ultrasound. While Prp is focussed on the insertion of the Achilles and the adjoining area of the tendon, the rest of the substance of the tendon and other adjacent calcaneal and malleolar attachments are subjected to comprehensive prolotherapy. We have seen excellent results with this treatment modality and believe should be a first line treatment offered to patients not responding top conservative means.
Surgery
Chronic cases not responding to non surgical means for more than 8-12 months are advised surgery. Surgeries for chronic Achilles tendonitis
Gastrocnemius recession with or without denridement( usually for cases with less than 50 % of the tendon involved)
Debridement with repair also augmenting it with a tendon transfer if needed is carried out usually when more than 50% of the tendon is involved.
depends upon the amount of damage to the tendon.
Rehabilitation is usually started with an Air cast walking boot following the procedure.
REFERENCES
- Alfredson H, Forsgren S, Thorsen K.et alGlutamate NMDAR1 receptors localised to nerves in human Achilles tendons. Implications for treatment? Knee Surg Sports Traumatol Arthrosc 20009123–126. [PubMed] [Google Scholar]
- Alfredson H, Thorsen K, Lorentzon R. In situ microdialysis in tendon tissue: high levels of glutamate, but not protoglandin E2 in chronic Achilles tendon pain. Knee Surg Sports Traumatol Arthrosc19997378–381. [PubMed] [Google Scholar]
- Hart D A, Frank C B, Bray R C. Inflammatory processes in repetitive motion and overuse syndromes: potential role of neurogenic mechanisms in tendons and ligaments. In: Gordon SL, Blair SJ, Fine LJ, eds. Repetitive motion disorders of the upper extremity. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1995247–262.
- Scott A, Khan K M, Cook J L.et alWhat do we mean by the term “inflammation”? A contemporary basic science update for sports medicine. Br J Sports Med 200438372–380. [PMC free article] [PubMed] [Google Scholar]