Introduction
Plantar fasciitis is one of the most common causes of heel pain, affecting individuals across all age groups. It is characterized by inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes. This condition can cause sharp, stabbing pain, especially during the first steps in the morning. At Alleviate Pain Clinic, we provide a multidisciplinary approach to manage plantar fasciitis effectively. Here are ten proven treatment options to address this debilitating condition.
Ultrasound-Guided PRP (Platelet-Rich Plasma) Therapy
Plantar fasciitis is one of the most common causes of heel pain, affecting individuals across all age groups. It is characterized by inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes. This condition can cause sharp, stabbing pain, especially during the first steps in the morning. At Alleviate Pain Clinic, we provide a multidisciplinary approach to manage plantar fasciitis effectively. Here are ten proven treatment options to address this debilitating condition.
Ultrasound-Guided PRP (Platelet-Rich Plasma) Therapy
USG Guided plantar fascia injection by Dr Shubha Hegde at Alleviate Pain Clinic

plantar fascia injection by Dr Wiquar Ahmed at Alleviate Pain Clinic, Bengaluru
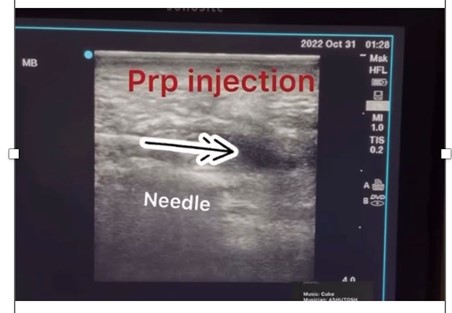
Plantar fasciitis can be challenging to treat, particularly when traditional methods fail. For chronic cases, Ultrasound-Guided Platelet-Rich Plasma (PRP) Therapy has emerged as an extremely promising , non-surgical treatment option. This regenerative injection therapy leverages the body’s natural healing potential to repair damaged tissues and alleviate pain.
How PRP Therapy Works
PRP therapy involves using your blood, which is processed to concentrate platelets—a rich source of growth factors critical for tissue repair. Platelets are known for their ability to:
- Stimulate the production of collagen, a vital structural protein in connective tissues.
- Promote angiogenesis (formation of new blood vessels), enhancing nutrient delivery to the plantar fascia.
- Reduce inflammation by modulating cytokines and other inflammatory mediators.
When injected into the affected area under ultrasound guidance, PRP is delivered precisely where it is needed, ensuring optimal therapeutic outcomes.
Benefits of Ultrasound Guidance
- Accuracy: Ultrasound imaging ensures the PRP is injected into the exact site of damage in the plantar fascia, avoiding unnecessary tissue injury.
- Real-Time Visualization: The clinician can monitor needle placement and tissue response in real time.
- Minimized Risk: Ultrasound guidance reduces complications, such as inadvertent injection into surrounding nerves or tissues.
Benefits of PRP Therapy for Plantar Fasciitis
- Non-Surgical: Unlike surgical options, PRP therapy is minimally invasive, reducing downtime and post-treatment discomfort.
- Stimulates Natural Healing: PRP harnesses your body’s intrinsic healing mechanisms, promoting tissue regeneration rather than merely masking symptoms.
- Reduced Dependency on Pain Medications: By addressing the root cause of inflammation, PRP reduces the need for long-term analgesic use.
- Long-Lasting Relief: Studies show that PRP therapy provides sustained pain relief and improved function over months.
Ideal Candidates for PRP Therapy
PRP therapy is particularly effective for:
- Chronic Plantar Fasciitis: Patients who have had persistent symptoms for more than six months and have not responded to conventional treatments like rest, physiotherapy, or corticosteroid injections.
- Athletes or Active Individuals: Those who wish to avoid surgery and recover quickly to return to their activities.
- Patients with Degenerative Changes: PRP is ideal for cases where imaging reveals thickened or degenerative plantar fascia.
- People Seeking Natural Healing: Patients looking for a treatment option without synthetic drugs or surgical intervention.
The Procedure
- Blood Draw: A small amount of your blood is drawn and processed using a centrifuge to isolate and concentrate platelets.
- Ultrasound Preparation: The plantar fascia is visualized using an ultrasound machine to identify the exact site of damage.
- Injection: PRP is injected into the plantar fascia under ultrasound guidance. A local anesthetic may be used to enhance comfort.
- Post-Injection Care: Patients are advised to avoid strenuous activity for a few weeks and may benefit from physiotherapy to optimize healing.
What to Expect After PRP Therapy
- Initial Soreness: Some patients may experience mild soreness for 24–48 hours due to the body’s inflammatory response to the injection.
- Gradual Improvement: Most patients notice significant improvement in pain and functionality within 4–6 weeks. Optimal results are often seen at 8–12 weeks as tissue healing progresses.
- Repeat Sessions: Depending on the severity, some cases may require 2–3 PRP injections spaced a few weeks apart.
Prolotherapy for Plantar Fasciitis
Prolotherapy is an innovative regenerative treatment designed to address chronic musculoskeletal pain, including plantar fasciitis. The procedure involves injecting a solution, typically a dextrose-based irritant, into the affected area to stimulate the body’s natural healing mechanisms. Here’s a closer look at its mechanism, benefits, and supporting evidence.
Mechanism of Prolotherapy in Plantar Fasciitis
Prolotherapy works by inducing a localized inflammatory response in the plantar fascia, which is the thick, fibrous band of tissue that supports the arch of the foot.
Triggering the Healing Cascade
- The injected solution causes mild irritation at the treatment site.
- This irritation signals the body to initiate a healing response, increasing blood flow and bringing growth factors to the area.
Collagen Production
- The inflammatory response stimulates fibroblasts (specialized cells) to produce new collagen.
- Collagen is essential for the structural integrity and strength of connective tissues like the plantar fascia.
Tissue Remodeling
Over time, the newly generated collagen integrates into the existing tissue, repairing microtears and strengthening the plantar fascia.
This regenerative approach not only addresses the symptoms of plantar fasciitis but also targets the underlying cause of tissue degeneration.
Benefits of Prolotherapy
- Non-Surgical and Minimally Invasive: Offers a viable alternative to surgical intervention for chronic cases.
- Promotes Natural Healing: Unlike symptomatic treatments, prolotherapy enhances the body’s own repair mechanisms.
- Long-Lasting Results: Strengthened plantar fascia reduces the likelihood of recurrence.
- Improved Functionality: Restores mobility and reduces pain during activities like walking or running.
Evidence Supporting Prolotherapy
Numerous studies and clinical trials highlight the efficacy of prolotherapy in treating plantar fasciitis:
- Improved Pain and Function Scores: A study published in the American Journal of Physical Medicine & Rehabilitation (2020) demonstrated significant reductions in pain and improvements in functional outcomes for patients with chronic plantar fasciitis who underwent prolotherapy.
- Comparison with Corticosteroid Injections: Research in the Journal of Foot and Ankle Surgery (2018) compared prolotherapy to corticosteroid injections and found that while both provided pain relief, prolotherapy offered longer-lasting results by promoting tissue healing rather than suppressing inflammation.
- High Patient Satisfaction Rates: A systematic review in Pain Medicine (2022) reported high satisfaction rates among patients who received prolotherapy, emphasizing its role as a preferred treatment for chronic, refractory plantar fasciitis.
- Safety Profile: Studies consistently report prolotherapy as a safe procedure with minimal side effects, making it suitable for a wide range of patients, including those unresponsive to conservative treatments.
Who Can Benefit from Prolotherapy?
- Chronic Plantar Fasciitis Patients: Particularly those who have not responded to physiotherapy, orthoses, or other conservative treatments.
- Athletes and Active Individuals: Seeking a treatment that restores function without prolonged downtime.
- Patients Avoiding Surgery: Prolotherapy offers an effective, minimally invasive alternative to surgical intervention.
Ozone Therapy for Plantar Fasciitis
Ozone therapy is an innovative and minimally invasive treatment option for plantar fasciitis. It utilizes a controlled mixture of ozone (O₃) and oxygen (O₂) to target inflammation and promote tissue regeneration in the affected plantar fascia. This cutting-edge approach has gained popularity due to its efficacy and safety profile.
Why It Works
Ozone therapy offers multiple benefits for plantar fasciitis due to its unique properties:
- Anti-Inflammatory Action: Ozone reduces inflammation by modulating the immune response, lowering pro-inflammatory cytokines, and reducing oxidative stress.
- Regenerative Potential: It stimulates cellular repair by enhancing oxygenation and encouraging the production of growth factors. This accelerates tissue healing and strengthens the plantar fascia.
- Improved Circulation: By boosting microcirculation, ozone ensures better delivery of nutrients and oxygen to the damaged tissue, facilitating recovery.
- Antimicrobial Effects: Ozone has antimicrobial properties, which can prevent or address infections if they are contributing to delayed healing.
Procedure
Ozone therapy is typically performed under ultrasound guidance to ensure accuracy and precision. The procedure involves the following steps:
Preparation
- The affected area is cleaned and sterilized.
- The patient is positioned comfortably to provide easy access to the heel and plantar fascia.
Ultrasound Imaging
- An ultrasound device is used to visualize the plantar fascia and surrounding structures.
- The inflamed or damaged areas are identified in real-time.
Ozone Injection
- A controlled mixture of ozone and oxygen is prepared at a specific concentration.
- Using a fine needle, the mixture is injected into the affected area with ultrasound guidance for precise placement.
Post-Procedure Care
- The patient may feel immediate pain relief or notice improvement over the next few days as the inflammation subsides and healing accelerates.
- Minimal downtime is required, and patients can usually resume light activities within 24 hours.
Advantages of Ultrasound Guidance
- Precision: Ensures the ozone is delivered directly to the inflamed or damaged tissue, avoiding unnecessary trauma to surrounding structures.
- Safety: Minimizes the risk of complications such as nerve or blood vessel injury.
- Efficacy: Increases the effectiveness of the treatment by targeting specific areas requiring intervention.
Corticosteroid Injections for Plantar Fasciitis
Corticosteroid injections are one of the most commonly used interventions for rapid pain relief in plantar fasciitis, particularly for patients experiencing severe or debilitating heel pain. These injections are designed to reduce inflammation and provide temporary relief, making them especially effective when other conservative measures fail to alleviate symptoms.
How Do Corticosteroid Injections Work?
Corticosteroids are potent anti-inflammatory medications that mimic natural hormones produced by the adrenal glands. When injected directly into the inflamed plantar fascia, they:
- Reduce Inflammation: By inhibiting pro-inflammatory pathways.
- Relieve Pain: By decreasing swelling and irritation in the affected tissue.
The effects are often noticeable within a few days and can last several weeks, providing a window of opportunity for patients to engage in complementary therapies like stretching and strengthening exercises.
Indications for Corticosteroid Injections
Corticosteroid injections are most appropriate for:
- Severe Pain: Cases where the pain significantly interferes with daily activities, such as walking, standing, or working.
- Chronic Conditions: When conservative treatments like physiotherapy, orthoses, or stretching exercises fail to provide relief after 6–12 weeks.
- Diagnostic Clarity: In cases of ambiguous heel pain, an injection can confirm that the plantar fascia is the pain source by providing temporary relief.
Procedure Details
- Pre-Injection Assessment: Ultrasound imaging is often used to locate the inflamed area accurately and guide the injection, ensuring precision.
- Injection: A small amount of corticosteroid, often mixed with a local anesthetic, is delivered directly into the painful area.
- Post-Injection Protocol: Patients are typically advised to rest and avoid high-impact activities for a few days to allow the medication to take effect.
Benefits of Corticosteroid Injections
- Quick Relief: Corticosteroids act faster than most conservative therapies, offering immediate symptom relief.
- Localized Treatment: Direct injection targets the inflamed tissue without systemic side effects.
- Improved Mobility: Reduced pain allows patients to participate in physical therapy or other long-term solutions.
Risks and Precautions
While corticosteroid injections can be highly effective, there are potential risks and limitations:
Overuse Risks
- Fascia Weakening: Repeated injections can weaken the plantar fascia, increasing the risk of partial or complete rupture.
- Fat Pad Atrophy: The fat pad on the heel may thin over time, reducing natural cushioning and potentially exacerbating pain.
Short-Term Effectiveness
Pain relief is often temporary, requiring other treatments for sustained improvement.
Infection
Though rare, any injection carries a minor risk of infection.
Tendon Damage
If administered incorrectly, corticosteroids may damage surrounding tendons.
Clinical Recommendations
- Frequency: Experts recommend limiting corticosteroid injections to a minimum to reduce the risk of complications like fascial rupture.
- Complementary Treatments: Combining injections with stretching exercises, orthotics, and physiotherapy ensures longer-lasting results.
- Patient Selection: This treatment is not recommended for athletes or individuals with acute plantar fascia injuries due to the risk of rupture.
Splints and Orthoses
Night Splints

Night splints are devices worn during sleep to keep the foot in a dorsiflexed position, gently stretching the plantar fascia and Achilles tendon. This prevents the fascia from contracting overnight, which is a common reason for the sharp, stabbing pain many people feel upon taking their first steps in the morning.
How They Work: By maintaining a prolonged stretch, night splints help to reduce morning stiffness and encourage healing of micro-tears in the plantar fascia.
Types:
- Posterior Splints: Cover the back of the leg and foot.
- Dorsal Splints: Wrap around the shin and top of the foot, offering a lighter, less restrictive option.
Usage Tips: Wear them for 6-8 hours during sleep for optimal results.
Custom Orthotic Insoles

Custom orthotic insoles are tailor-made inserts designed to support the arch of the foot and redistribute pressure across the sole. These are especially effective for individuals with biomechanical issues like overpronation (excessive inward rolling of the foot) or flat feet, which exacerbate strain on the plantar fascia.
Benefits
- Arch Support: Reduces excessive strain on the plantar fascia by providing structural support.
- Shock Absorption: Cushions the heel and absorbs impact during walking or running.
- Improves Alignment: Promotes proper alignment of the foot, ankle, and leg, reducing compensatory stress on other structures.
Who Should Use Splints and Orthoses?
These tools are highly effective for:
- Individuals with Biomechanical Imbalances: People with flat feet, high arches, or overpronation benefit the most.
- Patients Seeking Non-Invasive Options: Those who wish to avoid injections or surgical interventions.
- Chronic Pain Sufferers: Those experiencing persistent heel pain despite other conservative treatments.
- Active Individuals: Athletes or individuals engaged in prolonged standing or high-impact activities.
Additional Considerations
- Cost-Effectiveness: Orthotic insoles can be relatively affordable, especially compared to long-term therapies or surgical options. Custom versions, while pricier, often offer superior results and durability.
- Maintenance: Regular cleaning and replacement ensure optimal performance and hygiene.
- Combination Therapy: Night splints and orthoses work well when combined with stretching exercises, physical therapy, or regenerative treatments.
Physiotherapy Modalities for Plantar Fasciitis
Physiotherapy is a cornerstone of treatment for plantar fasciitis, offering non-invasive and evidence-based methods to reduce pain, enhance mobility, and promote healing. Among the most effective physiotherapy modalities are therapeutic ultrasound and extracorporeal shockwave therapy (ESWT), both of which target the affected tissues to accelerate recovery.
Therapeutic Ultrasound

Therapeutic ultrasound uses high-frequency sound waves to penetrate the plantar fascia and surrounding tissues, generating heat and vibration at the cellular level.
How It Works
The sound waves create a micro-massage effect that enhances blood flow and promotes the release of natural anti-inflammatory agents, reducing pain and swelling. The heat generated improves tissue elasticity and facilitates cellular repair.
Benefits
- Promotes deep tissue healing by stimulating fibroblast activity, which is critical for collagen repair.
- Reduces inflammation and associated pain.
- Relaxes tight tissues, improving flexibility.
Procedure
- A gel is applied to the skin over the heel and arch of the foot to enhance sound wave conduction.
- The ultrasound device is gently moved over the area for 5–10 minutes per session, depending on the severity of the condition.
- Sessions are typically conducted 2–3 times per week for 4–6 weeks.
Extracorporeal Shockwave Therapy (ESWT)

ESWT is a non-invasive treatment that delivers focused high-energy sound waves to the plantar fascia to address chronic pain and stimulate tissue repair.
How It Works
The sound waves cause controlled microtrauma to the tissues, triggering the body’s natural healing processes. This increases blood flow, breaks down calcifications, and reduces scar tissue that contributes to pain.
Types of ESWT
- Focused ESWT: Penetrates deeper tissues for severe cases.
- Radial ESWT: Targets superficial tissues and is effective for mild to moderate plantar fasciitis.
Benefits
- Accelerates tissue repair by boosting local circulation and encouraging angiogenesis (formation of new blood vessels).
- Reduces pain by desensitizing nerve endings and releasing natural pain-relieving chemicals like endorphins.
- Non-invasive with no downtime, allowing patients to resume daily activities immediately.
Procedure
- The affected area is marked, and a gel is applied for sound wave conduction.
- A shockwave applicator is placed over the heel, delivering short bursts of energy.
- The procedure typically lasts 15–20 minutes per session, with 3–5 sessions recommended over several weeks.
Side Effects
ESWT is generally safe, with mild soreness or bruising in the treated area being the most common side effect, which resolves in a few days.
Combination of Therapeutic Ultrasound and ESWT
When combined, these two modalities provide synergistic benefits:
- Ultrasound enhances tissue pliability, making the plantar fascia more receptive to shockwave treatment.
- ESWT builds on the groundwork laid by ultrasound, offering deeper repair mechanisms.
Stretching and Strengthening Exercises for Plantar Fasciitis
Stretching and strengthening exercises are essential for managing and preventing plantar fasciitis. These exercises improve the flexibility of the plantar fascia and surrounding muscles while strengthening the foot and lower leg muscles. This dual approach reduces strain on the fascia, promotes healing, and prevents recurrence.
Target Areas
- Plantar Fascia: The main tissue affected by plantar fasciitis, requiring gentle yet targeted stretching.
- Achilles Tendon: Tightness in this tendon increases tension on the plantar fascia, making it crucial to improve its flexibility.
- Calf Muscles: Tight calf muscles (gastrocnemius and soleus) often contribute to plantar fascia strain.
Detailed Examples of Effective Exercises
Toe Stretches

How to Perform
- Sit with your legs extended.
- Grab the toes of the affected foot and pull them gently toward your shin until you feel a stretch along the arch of your foot.
- Hold for 15–30 seconds and repeat 3–5 times.
Benefits
- Improves plantar fascia flexibility.
- Reduces morning stiffness and pain.
Calf Stretches (Standing Wall Stretch)

How to Perform
- Stand facing a wall, place both hands on the wall for support.
- Step back with the affected leg, keeping it straight with the heel on the floor.
- Bend the front knee while keeping your back leg straight to stretch the calf.
- Hold for 30 seconds and repeat 3 times per leg.
Benefits
Loosens tight calf muscles, reducing strain on the plantar fascia.
Towel Curls
How to Perform
- Place a towel flat on the floor and sit in a chair.
- Use your toes to grab and scrunch the towel toward you.
- Release and repeat for 10–15 repetitions.
Progression
Add a small weight (like a water bottle) to the towel for increased resistance.
Benefits
- Strengthens the intrinsic muscles of the foot.
- Improves arch support and reduces plantar fascia tension.
Plantar Fascia Stretch with Ball
How to Perform
- Place a small ball (e.g., tennis ball) under the arch of your foot.
- Roll the ball back and forth for 2–3 minutes while applying light pressure.
Benefits
- Loosens fascia tissue and improves blood flow.
- Reduces inflammation and promotes healing.
Toe Taps
How to Perform
- Sit with your feet flat on the ground.
- Lift only your toes while keeping the rest of your foot on the floor, then lower them.
- Repeat for 10–15 repetitions.
Benefits
Strengthens toe flexors and stabilizes the arch.
Seated Foot Stretch (with Strap)
How to Perform
- Sit on the floor with your legs extended.
- Wrap a resistance band or towel around the ball of your foot.
- Gently pull your foot toward you while keeping the leg straight.
- Hold for 15–30 seconds, repeat 3 times.
Benefits
Enhances plantar fascia and Achilles tendon flexibility.
Precautions
- Start Slow: Avoid overstretching, as this can worsen inflammation.
- Warm Up: Perform gentle warm-up activities like walking before stretching.
- Consistency: Daily practice is essential for long-term benefits.
- Avoid Pain: If an exercise causes sharp pain, stop and consult your healthcare provider.
Advantages of Stretching and Strengthening Exercises
- Prevention of Recurrence: Regular stretching and strengthening reduces tension in the fascia and surrounding structures.
- Enhanced Healing: Promotes blood flow to the plantar fascia, speeding recovery.
- Improved Foot Mechanics: Strengthened muscles provide better arch support, reducing strain.
- Cost-Effective: These exercises can be performed at home without special equipment.
Footwear Modifications
Choosing the right footwear is a cornerstone in managing plantar fasciitis. Inappropriate footwear can exacerbate heel pain by failing to provide adequate support, cushioning, and shock absorption. On the other hand, well-designed shoes and insoles can alleviate stress on the plantar fascia, aid in recovery, and prevent future flare-ups.
Why Footwear Matters
The plantar fascia acts as a natural shock absorber, supporting the arch of your foot. Shoes that lack arch support or cushioning can strain this structure, leading to inflammation and microtears. Correct footwear redistributes pressure, reduces stress on the fascia, and enhances comfort during daily activities.
Key Recommendations
Avoid High Heels
- Why They’re Harmful: High heels shift the body’s weight forward, increasing strain on the forefoot and plantar fascia. They can also shorten the Achilles tendon, which contributes to tension in the fascia.
- Alternative: Opt for shoes with a slight heel (around 1-2 inches) as completely flat soles can also cause problems.
Avoid Flat-Soled Shoes
- Examples of Problematic Shoes: Flip-flops, ballet flats, and minimalist shoes. These typically lack arch support, leaving the plantar fascia vulnerable to overuse.
- Alternative: Choose footwear with contoured footbeds that support the arch and cradle the heel.
Opt for Shock-Absorbing Insoles
- Benefits: Insoles with shock-absorbing materials (e.g., gel, foam, or memory foam) reduce the impact on the heel and provide additional cushioning.
- Custom Orthotics: For individuals with unique foot shapes or severe cases, custom orthotic insoles designed by a podiatrist can offer tailored support.
Look for Adequate Arch Support
- Why It’s Essential: Proper arch support prevents the fascia from overstretching, especially during long hours of walking or standing.
- Tip: Shoes labeled as “orthopedic” or “designed for plantar fasciitis” often incorporate robust arch support.
Ensure a Proper Fit
- Comfort Matters: Ill-fitting shoes can create pressure points and worsen symptoms. Always ensure there’s enough room in the toe box to allow natural foot movement.
- Break-In Period: If switching to supportive footwear feels uncomfortable initially, gradually increase wearing time to allow your feet to adapt.
Prioritize Durable Outsoles
Shoes with thick, durable outsoles can absorb impact and provide stability. Look for features like rubber soles and textured grip for additional traction and protection.
Specialized Footwear Options
- Athletic Shoes: Running or walking shoes with built-in cushioning and arch support are great options for everyday wear.
- Supportive Sandals: Brands like Birkenstock or Vionic offer sandals designed with orthopedic support for warm weather.
- Work Shoes: If you stand for long hours, choose work-specific shoes with features like padded insoles, wide toe boxes, and reinforced arches.
- Night Splints: Although not everyday footwear, these can be worn while sleeping to keep the plantar fascia gently stretched, aiding in recovery.
Lifestyle Modifications
Plantar fasciitis is often exacerbated by daily habits and lifestyle choices that place excessive stress on the feet. By making intentional changes, you can reduce strain on the plantar fascia, promote healing, and prevent future flare-ups. Below are some detailed lifestyle modifications to improve outcomes significantly.
Weight Loss to Reduce Foot Strain
Excess body weight increases the load on your feet, particularly the plantar fascia, during standing, walking, or running. Reducing weight can alleviate this pressure, minimizing inflammation and pain.
How It Helps
- Reduces mechanical stress on the arches.
- Improves overall biomechanics, reducing the risk of plantar fasciitis recurrence.
Tips for Implementation
- Adopt a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
- Incorporate low-impact cardio exercises like walking, cycling, or swimming to burn calories without straining your feet.
- Consult a nutritionist or healthcare provider for personalized weight-loss plans.
Avoid Prolonged Standing or Walking on Hard Surfaces
Extended periods of standing or walking, especially on hard, unforgiving surfaces, can overstress the plantar fascia, worsening pain and inflammation.
How It Helps
- Allows the plantar fascia to rest and recover.
- Minimizes repetitive microtrauma to the tissue.
Practical Adjustments
- Use anti-fatigue mats if your job requires standing for long periods.
- Take regular breaks to sit down and elevate your feet.
- Opt for cushioned footwear with proper arch support to absorb shock.
- Avoid walking barefoot on hard floors; wear supportive slippers indoors.
Incorporate Regular Low-Impact Activities
Staying active is essential for overall health, but high-impact activities like running or jumping can worsen plantar fasciitis. Low-impact activities provide the benefits of exercise without straining the plantar fascia.
Recommended Activities
- Swimming: Provides a full-body workout while taking all weight off your feet.
- Cycling: Strengthens lower leg muscles, which support the plantar fascia, without putting pressure on your heel.
- Yoga: Improves flexibility and strengthens muscles around the plantar fascia, reducing strain.
Tips for Success
- Gradually increase the intensity and duration of your workouts to prevent overuse injuries.
- Incorporate stretching exercises post-activity to keep the plantar fascia and surrounding muscles flexible.
- Choose soft, even surfaces for activities like walking or yoga to further reduce strain.
Surgery for Plantar Fasciitis
Surgery for plantar fasciitis is typically reserved as a last resort when conservative treatments, such as physical therapy, orthotic devices, regenerative therapies, and corticosteroid injections, fail to provide relief after 6–12 months. The most common surgical option is plantar fascia release, which involves cutting part of the plantar fascia to relieve tension and reduce inflammation.
Types of Surgical Procedures
Open Plantar Fascia Release
- A traditional approach where a small incision is made near the heel.
- The surgeon carefully releases the plantar fascia without compromising surrounding structures.
- Often used for cases with severe scarring or heel spur involvement.
Endoscopic Plantar Fascia Release (EPFR)
- A minimally invasive technique where a small camera (endoscope) and surgical tools are used.
- Allows for quicker recovery and reduced risk of complications.
Indications for Surgery
Surgery is considered when:
- Pain persists despite 6–12 months of conservative treatments.
- Activities of daily living are significantly impaired.
- Imaging studies, such as ultrasound or MRI, confirm chronic thickening, tearing, or other structural abnormalities in the plantar fascia.
Risks and Complications
While rare, complications can include:
- Nerve damage leading to numbness or tingling.
- Infection at the surgical site.
- Over-release of the plantar fascia, potentially destabilizing the foot arch.
A Multidisciplinary Approach at Alleviate Pain Clinic
At Alleviate Pain Clinic, we emphasize a comprehensive and patient-centered approach to plantar fasciitis. Our team combines cutting-edge interventional techniques, physiotherapy, and lifestyle counseling to address the root cause of the problem.
Why Choose Us?
- Expertise in ultrasound-guided regenerative treatments like PRP,prolotherapy and ozone treatments.
- Customized treatment plans including orthotic fittings and tailored physiotherapy treatment plans
- Access to advanced modalities like ESWT and therapeutic ultrasound.
- Clinical Nutrition – Optimizing weight and lessening the load on the plantar fascia.
By addressing all aspects of the condition, we aim to ensure long-term relief and improved quality of life for our patients.
Patient undergoing PRP treatment for plantar fasciitis at Alleviate Pain Clinic, Bengaluru Dr Roshan Adappa
References
- Ahmed AS, “Role of PRP in Chronic Plantar Fasciitis,” Journal of Regenerative Medicine,
- Rabago D et al., “Prolotherapy for Plantar Fasciitis: A Systematic Review,” Pain Medicine,
- Wang CJ et al., “Effectiveness of Shockwave Therapy in Plantar Fasciitis,” Journal of Orthopedic Surgery,
- Coombes BK et al., “Corticosteroid Injections for Plantar Fasciitis: A Meta-Analysis,” The BMJ,
- Singh D et al., “Impact of Footwear on Plantar Fascia Health,” Journal of Foot and Ankle Research,