Introduction
Joint Hypermobility Syndrome (JHS) is a condition that affects the flexibility and stability of the body’s joints, leading to a wide range of symptoms and discomfort. This comprehensive guide explores what Joint Hypermobility Syndrome is, differentiates it from general joint hypermobility, and discusses the relationship between JHS and Ehlers-Danlos syndrome. We will delve into the symptoms, causes, diagnosis, and management of JHS, with a special focus on Prolotherapy as a promising first-line treatment for this condition.
What is Joint Hypermobility Syndrome?
Joint Hypermobility Syndrome (JHS) is a connective tissue disorder characterized by the excessive flexibility of the joints. It is not a rare condition and can affect individuals of all ages. The primary feature of JHS is joint hypermobility, which often leads to musculoskeletal pain, joint instability, and a heightened risk of injury.
The Difference Between Joint Hypermobility and Joint Hypermobility Syndrome
While joint hypermobility is a term used to describe an increased range of motion in one or more joints, Joint Hypermobility Syndrome encompasses a broader clinical picture. JHS is characterized not only by hypermobile joints but also by a range of symptoms, including chronic pain, muscle weakness, and fatigue. Joint hypermobility itself does not necessarily lead to the other associated symptoms of JHS.
Conditions exhibiting joint hypermobility
- Ehlers-Danlos Syndrome (EDS) : EDS is a group of inherited connective tissue disorders that affect collagen production and function. It is often classified into several subtypes, each with its unique genetic basis and clinical characteristics. While joint hypermobility is a common feature of EDS, it can also involve other systemic issues, such as skin hyperelasticity, easy bruising, and vascular problems. EDS is primarily genetic, whereas JHS is typically acquired and may have an underlying genetic predisposition.
- Marfan Syndrome : Marfan syndrome is another genetic connective tissue disorder that shares some similarities with EDS but has distinct clinical features, such as skeletal abnormalities, cardiovascular issues, and eye problems.
- Down Syndrome : Down syndrome is a chromosomal disorder characterized by cognitive impairment and certain physical features. It is not directly related to joint hypermobility or connective tissue issues.
Symptoms of Joint Hypermobility Syndrome

The symptoms of Joint Hypermobility Syndrome can vary widely among individuals. Common symptoms and manifestations of JHS may include:
- Joint hypermobility, often with joint pain and instability.
- Chronic musculoskeletal pain, affecting multiple joints.
- Muscle weakness.
- Fatigue.
- Gastrointestinal issues, such as irritable bowel syndrome (IBS).
- Easy bruising and poor wound healing.
- Anxiety and depression, which are more prevalent in individuals with JHS.
Causes of Joint Hypermobility Syndrome
The exact cause of Joint Hypermobility Syndrome is not fully understood. It appears to result from a combination of genetic and environmental factors. Some individuals may have a genetic predisposition that makes them more susceptible to developing JHS. Additionally, factors like injury, repetitive joint overuse, or hormonal changes can contribute to the development or exacerbation of JHS symptoms.
Diagnosis and Tests
Diagnosing Joint Hypermobility Syndrome typically involves a combination of clinical evaluation and assessment tools. Healthcare professionals may use the following approaches to diagnose JHS:

- Clinical Evaluation : A thorough medical history and physical examination are essential for identifying hypermobile joints and associated symptoms. The Beighton Score, which assesses joint hypermobility in specific body areas, is often used.
- The Five-Point Hypermobility Questionnaire : This questionnaire, consisting of five questions related to joint hypermobility and other JHS symptoms, can help in the initial assessment.
- Can you now (or could you ever) place your hands flat on the floor with your knees straight?
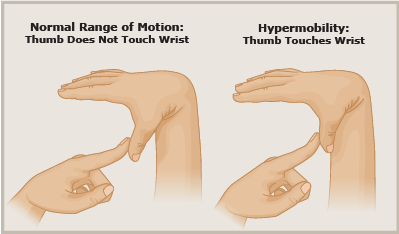
- Can you now (or could you ever) bend your thumb to touch your forearm?
- As a child, did you amuse your friends by contorting your body into strange shapes or could you do the splits?
- As a child or teenager, did your shoulder or kneecap dislocate on more than one occasion?
- Do you consider yourself double-jointed?
If you answered “yes” to two or more questions, you may have joint hypermobility syndrome.
- Beighton Score: The Beighton Score assesses joint hypermobility at various sites in the body. A score of 4 or more out of 9 is typically considered indicative of joint hypermobility.
- Genetic Testing: Genetic testing may be considered in cases where there is a strong family history of JHS or related connective tissue disorders.
Management and Treatment
How is Joint Hypermobility Syndrome Treated?
The management and treatment of Joint Hypermobility Syndrome aim to address the symptoms and improve an individual’s quality of life. Various approaches can be utilized:
- Physical Therapy : Physical therapy plays a crucial role in the management of JHS. Therapists can provide specific exercises to strengthen muscles, stabilize joints, and improve joint proprioception.
- Pain Management : Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), may be prescribed to manage pain and inflammation. In some cases, stronger pain medications may be necessary.
- Lifestyle Modifications : Lifestyle changes, such as modifying activities to reduce joint stress, can help manage symptoms. Using assistive devices like braces or orthotics may also be beneficial.
- Counseling and Psychological Support : The chronic pain and associated symptoms of JHS can have a significant psychological impact. Counseling and support from mental health professionals can help individuals cope with anxiety and depression.
- Prolotherapy as a First-Line Treatment : We at Alleviate Pain Clinic are big proponents of prolotherapy for joint hypermobility syndrome.Prolotherapy, or proliferation therapy, is a Regenerative Injection treatment that focuses on strengthening and repairing damaged ligaments and tendons. It is increasingly considered a first-line treatment for Joint Hypermobility Syndrome due to its regenerative properties. Prolotherapy involves injecting an irritant solution, often containing dextrose, into the affected ligaments and tendons. This initiates a healing response, resulting in the thickening and strengthening of connective tissues. The procedure is minimally invasive and is showing promise in improving joint stability and reducing pain in individuals with JHS.
Prevention
While Joint Hypermobility Syndrome is not preventable in the same way infectious diseases are, there are strategies to reduce the risk of developing JHS symptoms or to manage them effectively:
- Physical Activity : Engage in low-impact exercises and activities that help maintain muscle strength, joint stability, and joint proprioception. Physical therapy can provide tailored exercise programs.
- Joint Protection : Use protective gear or orthotic devices to reduce the risk of joint injuries during physical activities.
- Manage Stress : Stress management techniques and psychological support can help individuals cope with the psychological impact of chronic pain and other JHS symptoms.
Outlook / Prognosis
What Can I Expect If I Have Joint Hypermobility Syndrome?
The outlook for individuals with Joint Hypermobility Syndrome varies widely depending on the severity of symptoms, the effectiveness of treatment, and individual factors. While JHS is a chronic condition, many individuals can manage their symptoms effectively and lead fulfilling lives.
Prolotherapy is emerging as a promising first-line treatment for JHS, offering the potential to improve joint stability, reduce pain, and enhance overall quality of life. As research and clinical experience in this field continue to grow, individuals with JHS have reason to be optimistic about their long-term prognosis.
In conclusion, Joint Hypermobility Syndrome is a complex condition characterized by joint hypermobility and a range of associated symptoms. It differs from simple joint hypermobility and is not synonymous with Ehlers-Danlos syndrome. Early diagnosis, proper management, and the use of innovative treatments like Prolotherapy can significantly improve the quality of life for individuals with JHS. While it is a chronic condition, the prognosis is promising, and individuals can take steps to effectively manage their symptoms and enhance their well-being.